Written By Dr. Cheryl Burdette,
Director of Clinical Support & Education For Doctor's Choice

Cholesterol is a marker that has experienced changes in references ranges many times over the past 40 years. Much debate and discussion has focused on what it means when cholesterol is too high and what number is indicative of a level that is elevated. With so much focus on high cholesterol, the idea that cholesterol can be too low is often ignored. In fact, many laboratories have changed the way cholesterol is reported so instead of having a lower limit and an upper limit, e.g. normal range is equivalent to 140 to 200, you see shifts in this representation. It is quite common to see reference ranges of cholesterol reported as 0-200, indicating that the lower your cholesterol is the better. This is unfortunate and misleading. A cholesterol of zero is incompatible with life. To report this as normal is inaccurate at best. Functional reference ranges on Cardio profiles and the Functional Health Report from Doctor’s Choice avoid this critical short coming.
This patient’s Functional Health Report includes cardiovascular markers and so this concerning trend is not missed.
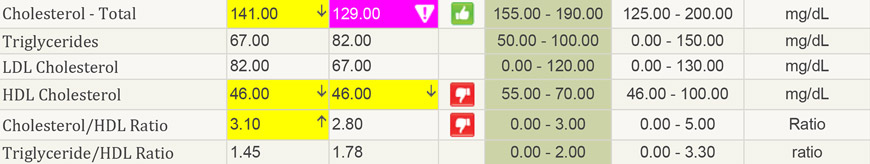
Cholesterol has fallen out of range. A standard reference range may report 0-200 as normal, or as in this case 125-200 as normal. However, research shows that a cholesterol of less than 155 is associated with an increased risk of suicide, depression, and hemorrhagic stroke. We know that cholesterol is necessary for many process in the body. It is the backbone for steroid hormones such as estrogen and testosterone. It is incorporated into every membrane to increase structural integrity. While it is true that too much cholesterol will create a rigid membrane that does not regulate cell health well, a membrane devoid of cholesterol will be too fluid, lacking the right balance of fats. Cholesterol is also necessary for creating bile, and so when it is low, you will see more problems with detoxification.
Low cholesterol in and of itself will cause symptoms, but we must always ask the question why it is low as well.
Some reasons for hypocholesterolemia include:
However, even though there are many causes, the thoroughness of the FHR helps with our differential diagnosis.
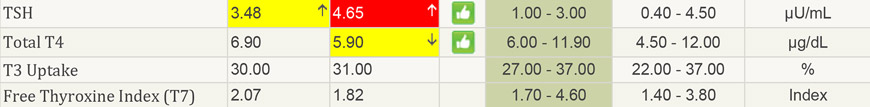
This demonstrates that hyperthyroidism is not an issue, and in fact, the opposite. The TSH is elevated, and T3 (Free Thyroxine Index T7), the most active thyroid hormone, is low normal. This would slow down the metabolism of cholesterol, making it higher, not lower, meaning despite a decrease in metabolism, this person is still experiencing low cholesterol.
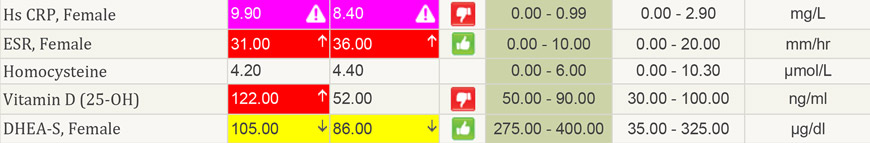
The next piece of information helps us to see their issue. This patient has a greatly elevated CRP and ESR. Both are markers of inflammation. When there is more inflammation, cytokines will be upregulated that can, when they are extreme, result in low cholesterol. A 2001 study in Critical Care showed that patients who had the highest levels of IL-6, IL-2 and IL-10 had the lowest cholesterol. Those with the lowest cholesterol had the worst outcomes in terms of survival. Low cholesterol is an indicator of poor health, and needs to be managed. However, for this patient, the best way to increase levels is not to increase fats in the diet or give Manganese for example, but to reduce the inflammation so that cytokines will fall and cholesterol production will normalize. Another sign that inflammation is at play is the decreased level of Vitamin D. The 25-OH form of Vitamin D is measured sequentially. When there is more inflammation there will be a hyper conversion of 25-OH Vitamin D to 1-25 Vitamin D which can cause levels to lower even without a decrease in intake. To further compound issues, DHEA is quite low, which helps to control inflammation. In a study that looked at DHEAs effect on insulin found that giving DHEA when women were low resulted in an improved insulin response as well as a decrease in cytokines, particularly IL-6. In this study 50mg of DHEA was given. This is certainly a high dose for women, and if levels like that were given, testing to monitor levels of DHEA would be warranted. (Aging (Albany NY). 2011 May;3(5):533-42.)
In my clinical observation, a dropping of cholesterol is a warning sign. While working at a cancer hospital, I found quite often, people with late stage disease had low cholesterol. Conventional reporting, increasingly, is not even recognizing that there is a low end to cholesterol. A Functional Health Report prevents missing highly meaningful and clinically relevant information. Using a functional range for cholesterol is not only supported by the research but provides a sharper clinical diagnosis and ultimately better patient care.